Sin Lee, a pathologist and scientist, believes the deck is stacked in the quest to air new ideas on Lyme disease.
Too many science journals telling him to take his research elsewhere. Too many deftly worded rejections. Too little inclination to engage in a fair fight over the facts and fiction of Lyme disease.
Dr. Lee’s experience is shared by many researchers I have interviewed, in the U.S. and Europe, in five years of writing about a disease on which scientific debate is limited and tightly controlled. Some
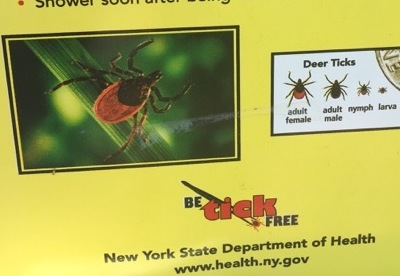
380,000 Americans were infected with the tick-borne spirochete in 2015, leaving 20,000, by conservative
estimates, with unresolved joint pain, cognitive lapses, fatigue and other problems. Another
232,000 are estimated to be infected annually in Western Europe. Many suffer because of a poor test and delayed diagnoses, issues that have been largely dismissed in mainstream journals.
Lee decided to take on some of the biggest names in Lyme disease, after their Dec. 15 publication of an
article, in Nature Reviews Disease Primers, that repeated the doctrines that have ruled Lyme disease care for nearly a generation. But his effort to rebut the article, centering on his call for better early diagnosis, was quickly squelched.
‘’Within days to weeks, [Lyme disease spirochetes] disseminate to other regions of the body or to other organs, the central nervous system, heart or joints.” — Steere article, which endorses waiting for a positive test to treat
“The point raised about requiring newer, better tests for diagnosis is undeniable, and the authors do discuss that,” Primers’ chief editor Mina Razzak wrote in a Dec. 20 email to Lee. “While I agree open dialogue and discussion is needed, this journal is not the best place for that...I am afraid we will not pursue publication of your letter.” Yes we agree there are problems, the editor was saying. Sorry, we won’t let you air them.
Lee, director of Milford Molecular Diagnostics, Milford, Connecticut, had other ideas, however. He posted his
challenge on PubMed Commons, an open-access alternative that allows comment by published scientists, where it appeared below the article abstract.
Sin Lee, a pathologist and scientist, believes the deck is stacked in the quest to air new ideas on Lyme disease.
Too many science journals telling him to take his research elsewhere. Too many deftly worded rejections. Too little inclination to engage in a fair fight over the facts and fiction of Lyme disease.
Dr. Lee’s experience is shared by many researchers I have interviewed, in the U.S. and Europe, in five years of writing about a disease on which scientific debate is limited and tightly controlled. Some
380,000 Americans were infected with the tick-borne spirochete in 2015, leaving 20,000, by conservative
estimates, with unresolved joint pain, cognitive lapses, fatigue and other problems. Another
232,000 are estimated to be infected annually in Western Europe. Many suffer because of a poor test and delayed diagnoses, issues that have been largely dismissed in mainstream journals.
Lee decided to take on some of the biggest names in Lyme disease, after their Dec. 15 publication of an
article, in Nature Reviews Disease Primers, that repeated the doctrines that have ruled Lyme disease care for nearly a generation. But his effort to rebut the article, centering on his call for better early diagnosis, was quickly squelched.
‘’Within days to weeks, [Lyme disease spirochetes] disseminate to other regions of the body or to other organs, the central nervous system, heart or joints.” — Steere article, which endorses waiting for a positive test to treat
“The point raised about requiring newer, better tests for diagnosis is undeniable, and the authors do discuss that,” Primers’ chief editor Mina Razzak wrote in a Dec. 20 email to Lee. “While I agree open dialogue and discussion is needed, this journal is not the best place for that...I am afraid we will not pursue publication of your letter.” Yes we agree there are problems, the editor was saying. Sorry, we won’t let you air them.
Lee, director of Milford Molecular Diagnostics, Milford, Connecticut, had other ideas, however. He posted his
challenge on PubMed Commons, an open-access alternative that allows comment by published scientists, where it appeared below the article abstract.
Come back in a few weeks
The 850-word comment argues that Lyme infections have been allowed, even encouraged, to fester. How? Under long-established guidance, repeated in the article, that physicians wait for a positive test before treating patients without the Lyme rash. Lacking a good early test, doctors thus tell non-rash patients who have wrongly tested negative — as 50 to 80 percent of early cases do, the paper admits — to return in awhile, giving the insidious Lyme pathogen time to grow. By then, in what is called the convalescent phase, many patients feel better and do not return, only to be
sickened later.
“The authors seem to advise the medical practitioners to not treat Lyme disease patients until the proliferating spirochetes in the host have elicited certain immune responses which can be confirmed by serologic tests,” wrote Lee, capturing the inexplicable logic of a flawed test. “Such practice should not be accepted or continued for obvious reasons.”
The article’s lead author was Allen Steere, who first
investigated the disease when it emerged in Connecticut in the 1970s. Others included Gary Wormser, lead author of controversial Lyme treatment
guidelines; Frank Strle, another guidelines author, and Paul Mead, an epidemiologist who has specialized in vector-borne diseases at the U.S. Centers for Disease Control and Prevention.
On behalf of the CDC, Mead disputed Lee’s critique. “CDC encourages prompt treatment of early Lyme disease. The suggestion that CDC is advising medical practitioners to withhold treatment until after the organism has disseminated is [his emphasis]
incorrect,” he wrote in an emailed statement. “The recommendations for serologic testing are for patients who
already have signs and symptoms suggestive of disseminated infection.”
Lyme disease can be diagnosed early, the CDC website states, ‘in patients who present with [a Lyme] rash.’ It does not say anything about people with symptoms but not the rash.
But patients have symptoms before the disease has disseminated, according to the CDC itself. Its website lists three symptoms of
“localized” — or not disseminated — infection: the rash, flu-like symptoms and swollen lymph nodes. However, the agency includes just one symptom to support diagnosis: “During the localized (early) stage of illness, Lyme disease may be diagnosed clinically in patients who present with [a Lyme] rash.” Not the flu, not abnormal lymph nodes.
CDC’s fine line
While the CDC’s website is carefully worded, the paper that Mead signed onto is crystal clear: “Demonstration of borrelial infection by laboratory testing is required for reliable diagnosis of Lyme borreliosis, with the exception of erythema migrans,” the name for the reddish Lyme rash.
In one venue, namely the article on which he is a co-author, Mead is unequivocal that only tests can diagnose early non-rash infection. In the other, he and the CDC walk a fine line, approving diagnosis for those with the rash, but silent on the rest.
I asked Mead whether the CDC agreed with the article’s contention that a positive test is “required” without the rash, which, a CDC
web page says, appears in 60 to 80 percent of cases. He noted that the article refers to “reliably” diagnosing, as opposed to treating, early disease, a distinction perhaps without a difference. He nonetheless left room for treatment based on symptoms.
With regard to empiric treatment of possible early Lyme disease,” he wrote, “clinicians should consider the patient’s signs and symptoms, the many other diseases that may produce similar symptoms (including other tickborne and non-tickborne infections), and the risks and benefits of presumptive antibiotic treatment.”
Read the entire article on Huffington Post.