
Learn about the impact of Lyme disease on sleep, Lyme disease insomnia, and how to manage sleep disturbances. Discover why Lyme disease causes sleep problems and find effective remedies to improve sleep quality.
I recently went out for a late dinner with friends. When the waiter came by with dessert menus, I glanced at my watch: 9:45 p.m. “I actually need to head out,” I said to the group. “You all stay and enjoy dessert, but I need to call Pumpkin Time.”
My friends laughed good-naturedly and bid me good night, knowing that like Cinderella, I need to keep a strict curfew and bedtime. For me, “turning into a pumpkin” means hitting a wall of neurological and physical fatigue, throwing off the circadian rhythm that I’ve worked so hard to re-establish since I was bitten by a tick more than two decades ago.
I’ve been in remission from Lyme disease and babesiosis, as well as chronic active Epstein-Barr virus, for more than a decade. When I do have flare-ups, though, the first thing to falter is my sleep, and suddenly it feels like the whole foundation of health I’ve built is crashing down. I’m all too quickly reminded of the very worst days of illness when sleep disturbances kept me awake for literally days on end, threatening my sanity. I never want to return to night upon night of raging insomnia, to hallucinogenic nightmares when I did sleep, to an inability to turn my brain off for a nap no matter how desperately tired I was during the day. Sleep disturbances were the very worst symptom of my tick-borne illnesses—beyond the migraine headaches, the joint pain, the fevers, the hives, and other physical and neurological symptoms—and now that my circadian rhythm is back, I protect it the way one might protect a retirement account.
Sleep disturbances are a real problem for many patients of neurological Lyme disease. Let’s walk through why that is, and perhaps more importantly, what you can do to manage them.
What is Neurological Lyme Disease?
When Lyme disease is caught and treated early, it usually stays localized, known as Stage 1 or early localized Lyme disease. At this point, Lyme disease bacteria (spirochetes) have not yet spread throughout the body. Left untreated, the illness can progress to Stage 2 (early disseminated) or Stage 3 (late disseminated) disease. When this happens, the spirochetes can cross the blood-brain barrier, a protective border of cells that form the walls of blood vessels that regulate what moves between the blood and the brain. Spirochetes are sneaky, and can spiral their way across this protective barrier, burrowing into the central nervous system. This causes neurological Lyme disease, which can manifest as brain fog, memory loss, peripheral neuropathy, word iteration, sensory overload, disorientation, and other cognitive impairment sometimes referred to as “Lyme brain”.
Why Does Lyme Disease Cause Sleep Disturbances?
Lyme is an inflammatory disease. When it crosses into the central nervous system, it causes nervous system inflammation, which literally alters the brain’s function and manifests as various impairments. As Robert Bransfield, MD explains in his lecture “The Assessment and Treatment of Sleep Disorders Associated with Lyme/Tick-Borne Diseases,” Lyme disease bacteria can attack the sleep center of the brain. This can cause a reversal of circadian rhythm, making patients wide awake when they’re supposed to be sleeping and exhausted when they’re supposed to be alert.[i]
Stay Connected, Make an Impact
Join our community of advocates by subscribing to our newsletter—stay informed with the latest breakthroughs in Lyme disease research and news. Ready to take the next step? Your donation to Global Lyme Alliance fuels the fight for a cure.
Subscribe Now to stay involved, or Donate Today to help us overcome Lyme disease.
How Does Lyme Disease Impact Sleep?
In his book How Can I Get Better? An Action Plan for Treating Resistant Lyme & Chronic Disease, Richard I. Horowitz, MD, says, “My patients either have problems falling asleep or complain of frequent awakenings during the night. They also complain of hypersomnolence: sleeping for twelve to fourteen hours. Yet, despite sleeping for long periods of time, they often report that they are still extremely fatigued.”[ii] This is exactly how I felt in my worst days of illness: bone tired all the time, but unable to fall or stay asleep. When I did get it, sleep was sometimes more exhausting than the excruciating waking hours, because I had so many fast-paced, crazy nightmares. My doctor said it was like the needle in my brain was stuck.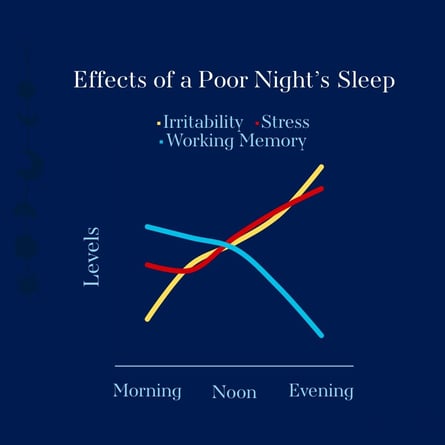
Without good sleep, my body was having difficulty battling infections. “Sleep deprivation is one of the primary reasons that you may remain chronically ill, because impaired sleep directly correlates with impaired immune function and, subsequently, inflammation,” writes Dr. Horowitz. “We even need proper sleep to clear toxins from the brain, so getting to the source of a sleep disorder is crucial, whether it is a direct effect of Borrelia burgdorferi and co-infections and/or due to overlapping medical problems, such as associated sleep apnea (affecting 22 million Americans), restless leg syndrome (RLS), mood disorders, medications, diet, nocturia (getting up to urinate), or hormonal dysregulation.”[iii]
What Helps Lyme-Related Sleep Disturbances?
The most important remedy for Lyme-related sleep disorders is adequate treatment of the Lyme disease infection, as well as any co-infections. Without proper antibiotic treatment, spirochetes will not be killed off and will continue to impact nervous system function. For the first two years that I was sick, I only had half a diagnosis of Epstein-Barr virus. While this diagnosis was accurate, I also had underlying tick-borne infections that were not being treated. Therefore, all the rest in the world and all of my efforts with over-the-counter sleep remedies did nothing to fix my sleep disorder, because the infections were only getting worse. Once I was on proper treatment, my sleep disturbances sometimes got worse due to Jarisch-Herxheimer reactions, but as spirochetes died off, my sleep problems died down.
Antibiotics alone did not quell my sleep disturbances, though. First, I had a sleep study to rule out other causes. It’s important to talk to your Lyme Literate Medical Doctor (LLMD) to see if you need a sleep study and to figure out what the best protocol is for correcting your sleep (unfortunately, there is no one-size-fits-all answer). For me, it was, and still is, very helpful to do neurofeedback, which uses the brain’s own feedback to train it to re-regulate itself. I also had to take various sleep medications at different points in my journey, and still take a regular non-narcotic medication that I will likely need long-term. Finally, I established good sleep hygiene, making sure my room was dark and quiet, using my bed only for sleep, getting up out of bed when I couldn’t sleep, and sticking to a strict sleep and nap schedule.
Over time, this combination, along with proper treatment of my infections, has moved me from surviving to thriving. I can’t control what the remaining spirochetes in my body will do, but I can give them the least chance possible of acting up, by sticking to good sleep hygiene—even if that means missing a piece of chocolate cake.
[i] Bransfield, RC. The Assessment and Treatment of Sleep Disorders Associated with Lyme/Tick-Borne Diseases John Drulle Memorial Lecture. 2016.
[ii] Horowitz, Richard I., MD. How Can I Get Better? An Action Plan for Treating Resistant Lyme & Chronic Disease. New York: St. Martin’s Press, 2017 (285).
[iii] Horowitz, Richard I., MD. How Can I Get Better? An Action Plan for Treating Resistant Lyme & Chronic Disease. New York: St. Martin’s Press, 2017 (286).
***

Jennifer Crystal
Writer
Opinions expressed by contributors are their own. Jennifer Crystal is a writer and educator in Boston. Her work has appeared in local and national publications including Harvard Health Publishing and The Boston Globe. As a GLA columnist for over six years, her work on GLA.org has received mention in publications such as The New Yorker, weatherchannel.com, CQ Researcher, and ProHealth.com. Jennifer is a patient advocate who has dealt with chronic illness, including Lyme and other tick-borne infections. Her memoir, One Tick Stopped the Clock, was published by Legacy Book Press in 2024. Ten percent of proceeds from the book will go to Global Lyme Alliance. Contact her via email below.
